What it IS
The patient-centric revenue cycle considers the patient's experience throughout the billing process. This includes an upfront understanding of the cost and transparent and timely communication regarding the balance due and payment options.
What it ISN'T
Perhaps to better understand what patient-focused revenue cycle elements include, it helps to identify what characteristics are not patient-focused but have been the standard for many years.
- Unclear pricing information for services.
- Unclear billing statements that do not articulate the insurance payment from the patient's responsibility.
- Lingering bills due to insurance denials, and some ultimately falling to a patient's responsibility.
- Lack of options for flexible payment plans and financing for patient balances.
Why Now?
Historically, the revenue cycle has not included a focus on the patient experience. Because the lion's share of the payments came from the insurance payors, the focus was to generate a claim that would elicit full payment on the first pass. For many years this was enough to keep hospitals financially sound. As patient pay responsibilities continue to rise, it has become increasingly critical to focus on the patient's experience with receiving the bill and their ability to pay. After all, the patient experience begins when they schedule their service, extending through to receipt and payment of the invoice. Patient satisfaction supersedes simply the evaluation of the service rendered. The new criterion includes: how easy was it to understand the cost upfront? Were financing options available? Were there any unexpected costs?
How to Create a Patient-Centric Revenue Cycle
Where to Start?
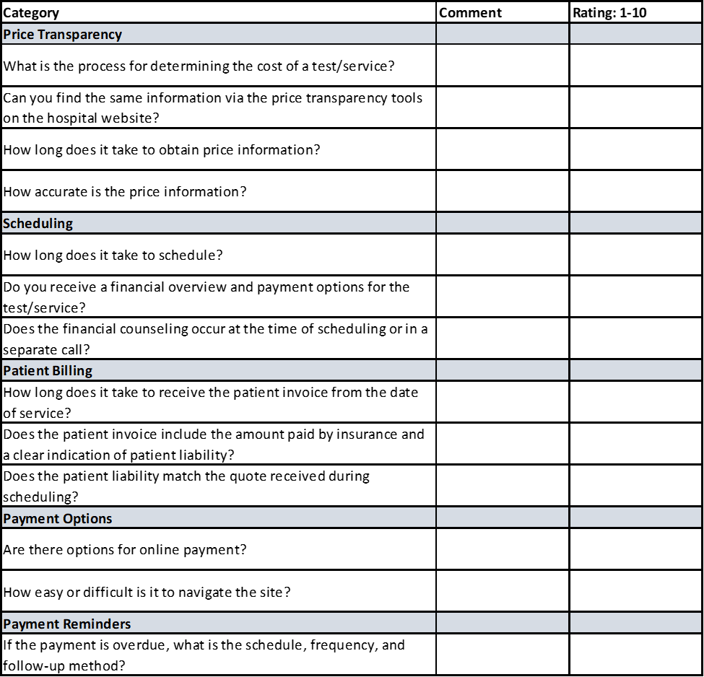
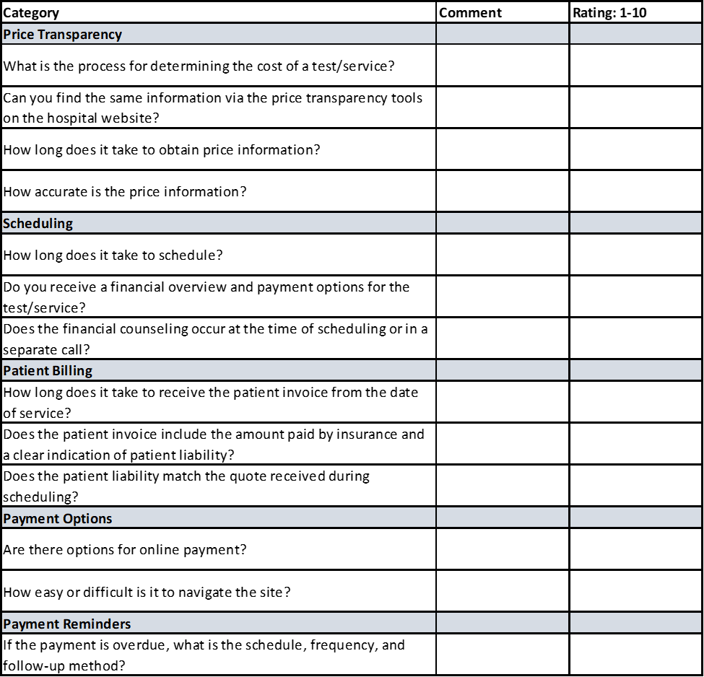
The best place to begin is in the shoes of the patient. Some of the best leaders test out their customer journeys by ascertaining services or participating as secret shoppers. Begin by creating a customer journey map and itemize the steps in the process so you can rate them on a scale from 1-10.
Recommendations for Improvement
Once you have evaluated this process, look for the places where the patient may be left uncertain or put forth an additional effort. What improvements can enhance the experience? By assessing opportunities for improvement in financial counseling, bill accuracy and understandability, and payment methods, direct and indirect benefits can arise. Increased patient satisfaction will retain and grow your patient base, and timely payment will reduce days in A/R.
Healthcare consumers in most locations have options and resources to seek the best outcomes and value for their money. Improvements to the revenue cycle can, directly and indirectly, impact patient satisfaction.
Discover What’s Holding Your Organization Back
MedCom Solutions provides a unique combination of clinical expertise and proprietary technology to help medical service providers meet rapidly escalating and changing medical billing demands.
Our Chargemaster, Pricing, and Compliance solutions have yielded hundreds of millions in net revenue for healthcare providers across the country.
Learn more about our solutions or visit our homepage or contact us today!