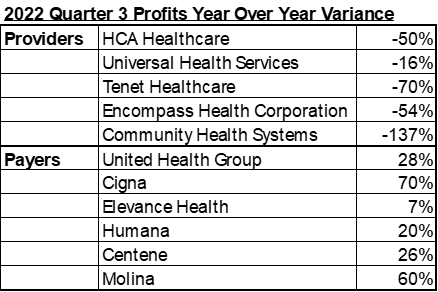
According to Becker's Healthcare, as of Quarter 3 of 2022, "economists have classified 2022 as the worst financial year for hospitals in decades," as the profit gap between payer and provider continues to widen.
Figure 1.1
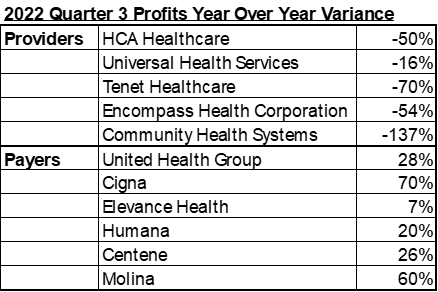
Note. Adapted From "'The house always wins': Insurers' record profits clash with hospitals' hardship" By Becker's Healthcare, 2022, https://www.beckerspayer.com/payer/the-house-always-wins-health-systems-face-worst-finances-in-decades-as-payers-rake-in-record-profits.html
The New Cost of Care
Annual Medicare payment adjustments do not typically meet the average service cost; therefore, it is left to the commercial payers to subsidize this gap. With costs increasing at historical rates, providers are working to balance their finances in any way possible.
At the same time, providers are spending more to get a single claim paid correctly. Across the country, roughly 30% of insurance claims submitted are either denied, lost, or ignored, according to DrCatalyst.com. Nearly 1/3 of the claims submitted will require additional efforts and resources to receive payment.
Staff salaries have increased, in addition to the time and effort required to submit a bill for accurate reimbursement. Not factoring in the increase in materials and utilities, the cost of providing care has changed.
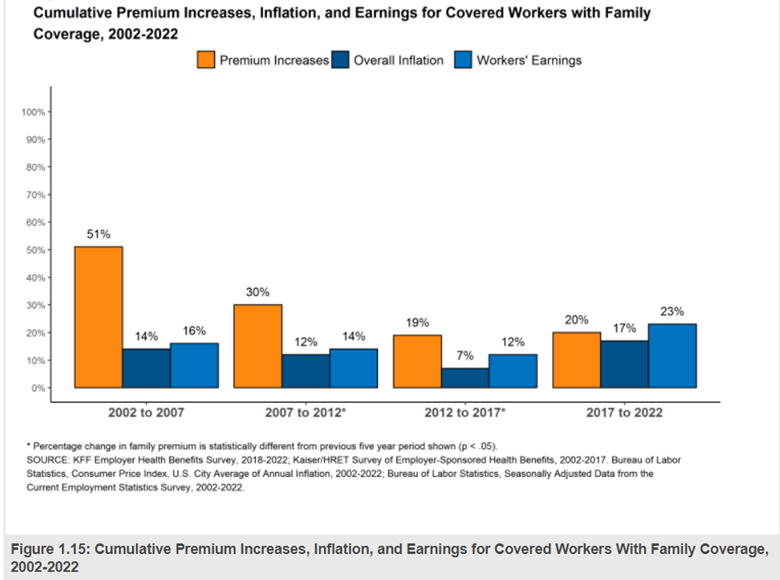
Health Insurance Premium Increases
Health insurance premiums increase yearly at a rate that exceeds earnings and inflation. "The $22,463 average family premium in 2022 is 20% higher than the average family premium in 2017 and 43% higher than the average family premium in 2012. The 20% family premium growth in the past five years is similar to the 19% growth between 2012 and 2017 […] This significant jump in inflation brings the growth in the average premium for family coverage over the last 5 years much closer to the rate of inflation over the same period (20% vs. 17%). The growth in the average premium for family coverage still outpaces the rate of inflation over the last ten years (43% vs. 25%)."
Figure 1.2
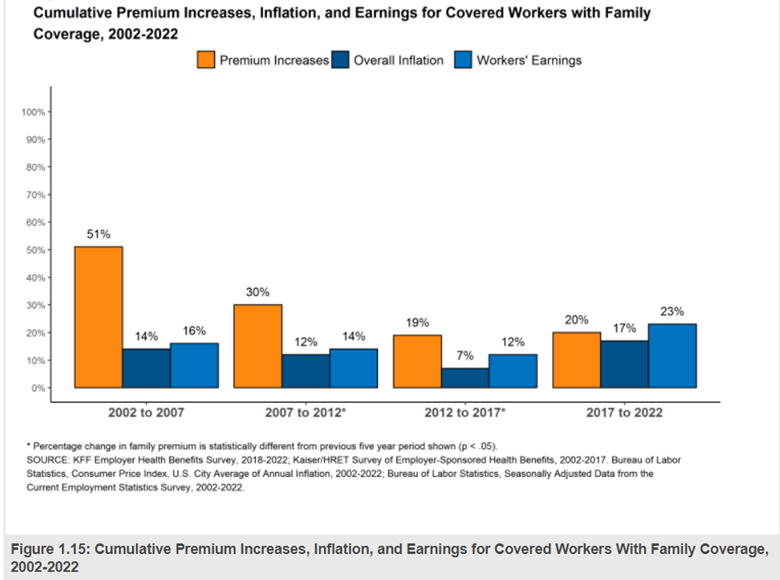
Note. KFF 2022 Employer Health Benefits Survey Section 1: Cost of Health Insurance, 2022, https://www.kff.org/report-section/ehbs-2022-section-1-cost-of-heatlh-insurance
So if payers have been increasing premiums at an average rate that exceeds earnings and inflation for the past 20 years, they should indeed have the means to adjust payment for services when costs rise. Yet, nationwide payer-provider negotiations are not going well. Providers elect to go out of network until renegotiations with reasonable terms are met.
How Successful are your Payer Negotiations?
If your system is like most in the US, you will likely meet resistance during payer contract negotiations. Some providers cannot even get the payer to schedule a meeting time. Once the talks begin, few go the way the provider hopes or needs. However, some providers see success when entering into renegotiations. What are these providers doing differently?
Keys to Successful Outcomes
- Positive Communication – while negotiations can become contentious, it's true that you "catch more flies with honey than with vinegar." Maintaining a positive relationship with your payer representative makes you more likely to see progress. But remember, you can be firm at the same time.
- Maintain Predictability – establish a rhythm of Communication with your payer representative before, during, and after negotiations. Regular Communication builds rapport and reaffirms to your payer that you are watching all payments and will follow up with them when you see inconsistent activity.
- Data-Driven is Best – use data to frame and seek what you ask. You don't necessarily need to show all the data you have. Key points will show that you have done your homework and know what you requested.
- Lofty and Realistic Goals – ask for everything but know where you are willing to concede. Model this data to measure the impacts of the decisions you need to make. Expect that you will be met with resistance but hold firm to what you need for a successful negotiation.
- Look at the Big Picture – remember that several factors impact the speed and accuracy of reimbursement. Contract negotiations should focus on payment rates and terms that might delay payment or add to the administrative burden.
Where to Start
If you don't have one, start assembling a cross-functional team to discuss pain points in the billing and accounts receivable process. By understanding where payment delays or denials occur, or additional documentation and administrative work are required, you can better understand the mounting cost of getting a single claim paid.
Performing a market analysis of your rates versus peers and payor reimbursement will provide a basis for areas where you may want additional pay increases.
At MedCom, we understand that many providers just don't have the time or resources to perform the necessary analyses for successful discussions and negotiations. With the support of the MedCom team, you can maximize your organization's efficiency and take control of your charge systems and processes.
MedCom offers a variety of customizable Charge Capture services, including Chargemaster, Pricing, and Order Entry Reviews, along with state-of-the-art affordable Software solutions.
Learn more about our solutions, visit our homepage, or contact us today!